WELCOME TO MY SITE
INTRODUCTION
PLEASE DO . GIVE ME YOUR FEED BACK AT tauqeeralibutt@apniisp.com OR tauqeeralibutt2004@yahoo.com OR mrbutt786@hotmail.com OR tauqeeralibutt@gmail.com OR tauqeer@tauqeeralibutt.20m.com
BLOOD TYPING
Definition:
Blood typing is a test to classify blood by determining the absence or presence of antigens on the red blood cells and the presence or absence of antibodies to these antigens in the serum.
Alternative Names:
Cross matching; Rh typing; ABO blood typing
How the test is performed:
Blood is drawn from a vein, usually from the inside of the elbow or the back of the hand. The puncture site is cleaned with antiseptic. An elastic band is placed around the upper arm to apply pressure and cause the vein to swell with blood.
A needle is inserted into the vein, and the blood is collected in an air-tight vial or a syringe. During the procedure, the band is removed to restore circulation. Once the blood has been collected, the needle is removed, and the puncture site is covered to stop any bleeding.
In infants or young children:
The area is cleansed with antiseptic and punctured with a sharp needle or a lancet. The blood may be collected in a pipette (small glass tube), on a slide, onto a test strip, or into a small container. A bandage may be applied to the puncture site if there is any bleeding.
How to prepare for the test:
The ABO typing process has 2 steps: forward and reverse typing. Initially, your blood is mixed with anti-A serum (serum that contains antibodies against type A blood), then with anti-B serum (serum that contains antibodies against type B blood). A determination of the blood type is based on whether or not the blood cells stick together (agglutinate) in the presence of these serums. The blood cells can stick together only when the anti-A antibody binds to the A antigen or the anti-B antibody binds to the B antigen. A laboratory technician can see the cells sticking together when the blood and serum are mixed in a test tube.
The second step involves placing your serum (the liquid portion of the blood without the cells) with blood that is known to be type A and type B (AB). With the results of these two steps, your blood type can be determined accurately.
Rh typing is similar to ABO typing. Here, your blood is mixed with serum containing anti-Rh antibodies and then observed for agglutination. If this occurs, you have Rh-positive blood. If the blood cells do not stick together, you have Rh-negative blood.
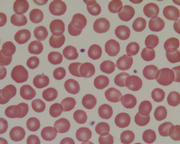
RED CELL ANTIGENS
The surface of the red cell consists of a bilipid membrane in which large protein molecules are embedded. The shape of the cell, along with its deformability, is maintained by skeletal proteins lying on the internal side of the bilipid layer. Haemoglobin fills the space surrounded by this complex membrane. The biconcave dist shape of the red blood cell maximizes the cell surface area.
The bilipid membrane is composed of a class of molecule called phospholipids. Phospholipids are amphipathic; that is, they have properties which are both hydrophilic and hydrophobic. The polar heads of the molecule are hydrophilic and the hydrocarbon tails are hydrophobic. It is natural for phospholipids to form sheets or bilipid layers with the hydrophobic tails of each molecule sequestered with in the bilipid layer. The hydrophilic heads are on the two surfaces of the bilipid layer-one surface exposed to the surrounding plasma while the other is exposed to hemoglobin. The membrane is symmetric in that certain phospholipids dominate the outer layer and others are predominantly on the inner layer. The membrane is described as fluid because the lipid molecules actively migrate within the membrane parallel to the surface. they very rarely "flip flop" from the outside to the inside or vice versa. This fluidity can be illustrated by showing that when two cells are fused their membranes completely integrate within about one hour.
Most of the protein molecules in the bilipid membrane have oligosaccharides attached in very precise positions. Oligosaccharides are groups of sugar molecules. Some of these are known to be blood group antigens. Others serve as sites for metabolic functions of the red cell but have no recognized blood group specificity.
The most important blod group antigens are A, B and D (Rho). A and B antigens are well defined chemically. The antigenic determinants are the terminal sugars of oligosaccharide chains attached either directly to the cell membrane or attached to protein chains which protrude from the bilipid layer. XWhen the oligosaccharide chains are attached to the cell membrane, the structure is called a glycolipid molecule, and when oligossacharides are attached to a protein structure, the molecule is called a glycoprotein, The Rh antigens are much well less defined but they are primarily protein and appear to be embedded in the bilipid membrane with the portions of the molecule exposed on the outer surface of the cell. They are probably associated with one of the protein chains in the membrane which has already been partially characterized.
The structure of all erythrocyte antigens in under genetic control. If a particular gene is inherited, the corresponding antigen is assembled and inserted into the membrane. Often a group of genes works in concert to produce a particular red blood cell antigen. The process of antigen of antigen production occurs during red blood cell maturation in the bone marrow prior to the loss of the red cell nucleus.
THE ABO SYSTEM
Importance of ABO Grouping
ABO grouping system is the most important test in medical laboratory and blood banking system, performed both on transfusion recipients and blood donors. The critical nature of ABO grouping stems from two characteristics of the system. First, unlike other blood group systems, antibodies of the ABO system are present in the serum of almost every person who does not have the corresponding antigen. Second, the all agglutinins of the ABO system fix complement and are capable of causing intra vascular hemolysis of incompatible red cells. For these reasons, an error in ABO grouping of a patient or donor could be fatal in a transfusion setting. While the cross-match affords an additional measure of protection, this may not be done in every case.
Tests Used To Determine A Person's ABO Group:
Accurate determination of a person's ABO group requires two different test procedures: red cell grouping also called as forward grouping and serum grouping also called as reverse grouping. The individual is first assigned to one of the four ABO blood groups - A, B, AB and O based on the reaction of red cells with blood grouping sera Anti-A and Anti-B. Blood grouping sera Anti-A and Anti-B are prepared from the sera of group B persons and group A persons. Anti AB serum prepared from specially selected group O individuals is not a simple mixture of Anti-A and Anti B but is the component of group O serum that has the special property of reacting with weak antigens on the red cells, especially weak A antigens. For this reason Blood Grouping Serum Anti AB is used routinely in some laboratories. In others, it is used only for special testing. Anti AB, serum will agglutinate group A, B and AB but will not agglutinate cells of O. This is especially important when testing with donor units to prevent mistyping a weak sub-group and labeling the unit group O. Anti AB serum should always be included in resolving discrepant results between cell and serum grouping.
Assuming that the tests are performed properly, visible interaction with antiserum indicates that the cells posses the antigen against which the antiserum is directed. Conversely no interaction indicates that the cells lack the antigen.
Following or simultaneously with red cell grouping, the serum of the individual is tested with known group A and B red cells to demonstrate the presence or absence of anti A and/or anti B. Because of the similarity in structure between A and B antigens of red cells and antigens of bacteria and plants, virtually every one who lacks either one or both of the antigens A and B produces antibody to the foreign antigen. Antibodies produced as a result of exposure to antigens of bacteria and plants are not observed until four to six months of age. The anti-A and B found in the serum of newborns is of maternal origin. The expected regularly occurring anti A and/or anti B, found in the serum of all people expect those of group AB, afford an ideal check on the red cell group. It is desirable to use A1 cells for maximum reactivity of the regularly occurring Anti-A in group B and group O sera. Some workers use A2 in addition to A1 cells.
RETICULOCYTE COUNT
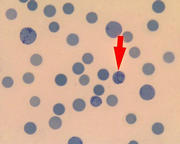
Reticulocyte Count
Reagents, Equipment
1. New Methylene Blue - Vital Stain
2. Microscope Slides
3. 12 x 75 test tubes
4. Applicator sticks
5. Beral pipettes
6. Timers
Procedure
1. Using a Beral pipette, place 5 drops of blood in the test tube.
2. Add 5 drops of New Methylene Blue stain to the test tube.
3. Mix and allow the mixture to stand at room temperature for 10 minutes.
4. Prepare at least 3 good smears and let them air dry.
5. Using the oil immersion lens count 500 red cells on one slide. Use the hand tally counter and a differential counter to record the number of reticulocytes counted as well as the total number of red cells counted. Be sure to include the reticulocytes in the total red cell count. Record the number of retics counted. Repeat this step with the other slide.
6. Calculate as follows:
Add together the total number of reticulocytes for the two slides. This yields the number of retics per 1000 RBC's. To convert to % divide this number by 10. For example, 10 retics on slide 1 and 15 retics on slide 2 equals 25 retics total or 2.5%.
Interpretation of Results
Normal Ranges
Adult: 0.5 - 1.5%
Newborns: 0.5 - 8%
Reticulocyte count is representative of bone marrow condition
1. RBC production increased, Retic count increases
2. RBC production decreases, Retic count decreases
Disease states with increased Reticulocyte counts
1. Hemolytic Anemias
2. After acute hemorrhage
3. Pernicious Anemia or iron deficiency anemia after treatment
Disease states with decreased Reticulocyte counts
1. Aplastic Anemia
2. Iron Deficiency Anemia before treatment
3. Pernicious anemia before treatment
If no retics are seen in 500 cells, both slides should be scanned for retics. If a retic is found on scan report retic count as <0.1%. If no retics are seen, set it up again, and if no retics are seen on the new slides then report as no retics seen on smear.
BLEEDING TIME
BLEEDING TIME
This is a test that measures the speed at which small blood vessels close off to stop bleeding (the condition of the blood vessels) and platelet function.
.First described by Milian in 1901 (8,9,10)
Duke observed duration of bleeding from small incisions of the ear lobe (1)
Two methods most widely used are the Ivy (2) and the template methods (3)
Principle:
Standard incision on volar aspect of forearm
Time the incision bleeds is measured
Cessation of bleeding is dependant on adequate number of platelets and of the ability of platelets to adhere to the subendothelium and to form aggregates.